The National Supplementary Health Agency (ANS) acts as a regulator of health plans in Brazil. Its main function is to create standards for this sector, control and monitor the companies that offer the plans. As it is linked to the Ministry of Health, its role is to ensure public interests in the face of the companies' actions.
One complaint to ANS should be made when a consumer feels harmed in some way during the provision of services. This can happen for several reasons, such as difficulties in coverage, billing errors, among others. If any of these situations occur and cannot be resolved directly with the company offering the plan, the ANS can be contacted.
How to make a complaint to ANS?
The first thing to do when a customer wants to resolve an issue regarding the provision of a service is to contact the SAC (Customer Service) of the company responsible for the plan.
With the enactment of Decree No. 6,523/2008, insurance companies are required to offer this service channel free of charge to their customers 24 hours a day.
It is important to note down the protocol number generated during the service, it will serve as proof in the following steps, if the problem continues to occur.
The rules also establish that from the moment of the complaint, companies have up to 5 days to present a solution. If this does not happen, the next step is to seek out the company's ombudsman.
Although they are part of the structures of the insurance companies themselves, ombudsman offices are bodies that represent the rights of customers. After a complaint is filed, the ombudsman office has up to 7 working days to provide a response to customers.
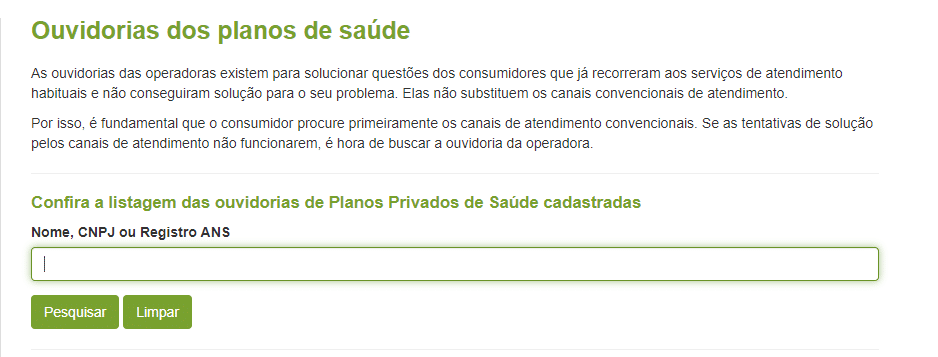
The ANS website itself offers a list of the ombudsman's office data for insurance companies registered in Brazil. Simply choose the Plans and Operators>Consumer Area>Consumer Service Center>Plan Ombudsman's Offices option from the home page.
These steps that must be followed before seeking a legal solution are important for consumers. Through the protocol numbers generated in these prior services, it is easier to prove in court that the customer's complaint is legitimate.
If policyholders have not found the expected solution in previous attempts, it is time to seek assistance from ANS.
On the “Customer Service Center” page, interested parties can view, in addition to the contact details of the companies’ ombudsman offices, the “ANS Hotline” number, a free channel through which they can speak to an agency attendant. The number is 0800 7019656.
For those who wish to file a complaint online, there is the “Contact Us” option. By clicking this button, the user will be redirected to the “Requestor Area”.
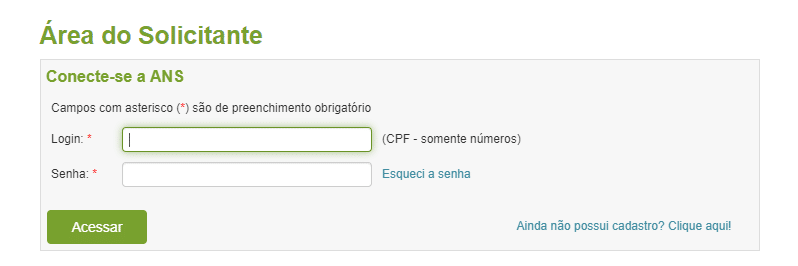
On this screen, you will be asked to provide information from people who are already registered on the ANS website. Those who are not registered should choose the option that appears in the bottom right-hand corner.
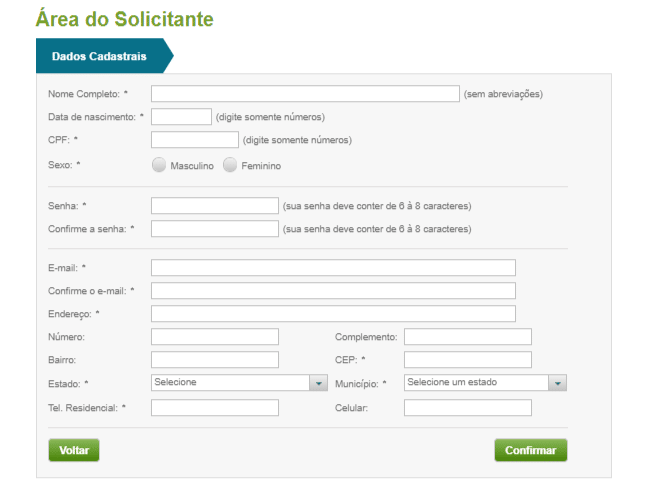
After completing the registration, you must return to the previous screen and log in.
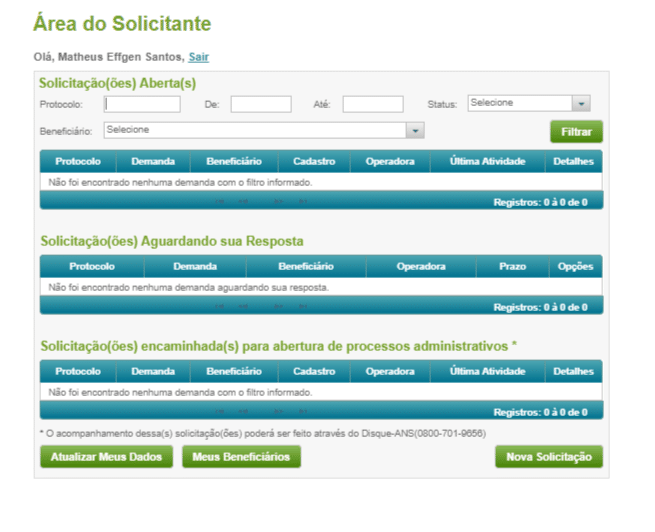
In this section, the customer must select the “New Request” option, located at the bottom right of the screen. Before this, the website already shows a series of preliminary information about recurring situations.
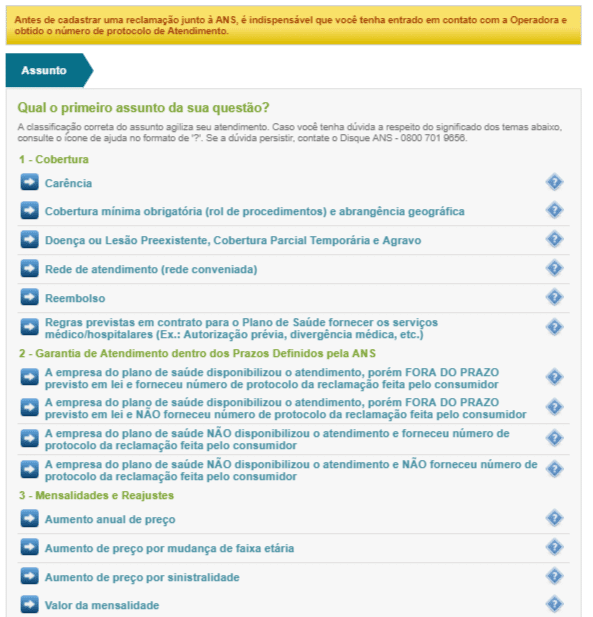
Then, all the options that can generate a complaint will be shown, just select one.
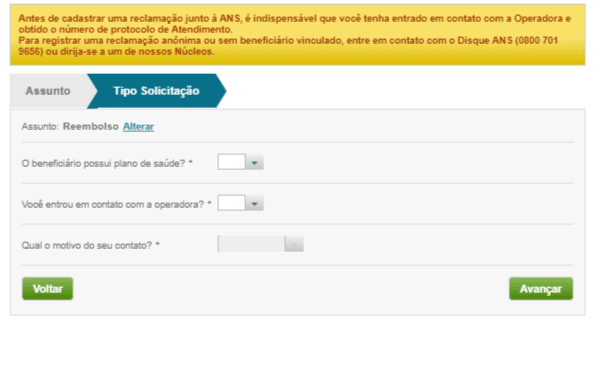
In this section, the most basic information about the request will be confirmed. It is not necessary to present a protocol as companies do not always provide one.
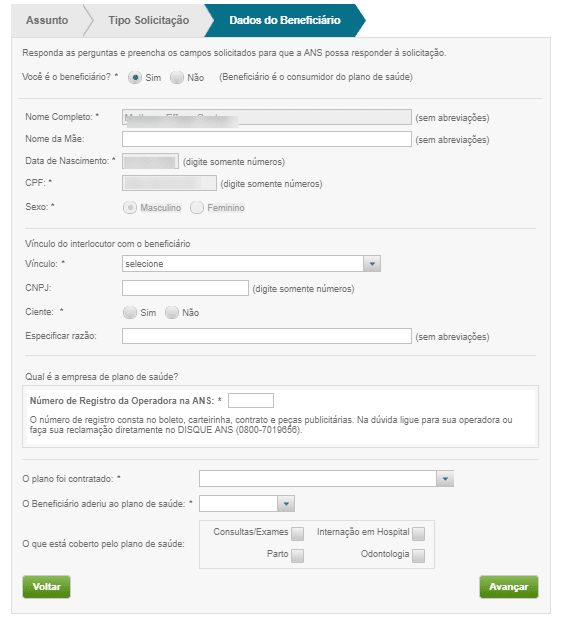
Here, details about the insured and the company offering the plan will be specified. The “ANS Operator Registration Number” can be found on the ANS website.
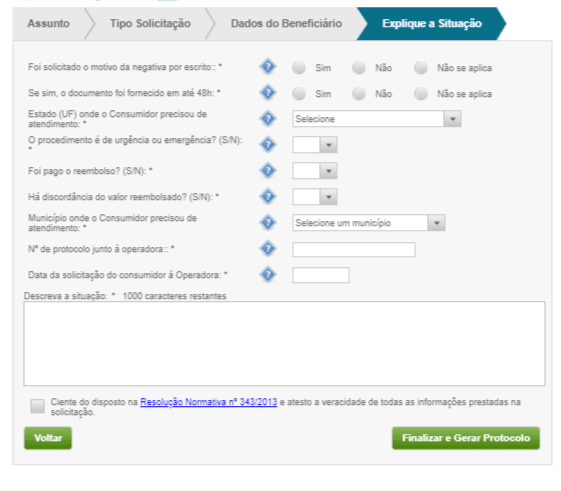
In the last form, the user must provide information that clarifies how the service was provided and will also describe the situation. In case of doubts, it is advisable to consult Normative Resolution No. 388/2015 on complaints to the ANS.
After that, simply select the option “Finalize and Generate a Protocol” and continue tracking the request through the website.
If the customer is dissatisfied with the response provided by ANS, the last resort is to file a lawsuit.



